The tonsillar fossa, posterior faucial pillars, and the base of the tongue are embryologically derived from the oropharyngeal brachial arches. The anterior faucial pillar and the retromolar trigone are embryologically connected to the oral cavity. [ref: 22] Although tumors that originate in the palatine arch share biologic behaviour with lesions of the oral cavity and some of the oropharynx, it is preferable to classify the tumors of the soft palate, anterior faucial arch, and retromolar trigone with oropharyngeal malignancies. [ref: 22] In the faucial arch the following well-defined structures are included: anterior tonsillar pillar, retromolar trigone, soft palate and uvula, glossopalatine (glossopharyngeal sulcus), and posterior tonsillar pillar.
The oropharynx can be subdivided into the palatine (faucial) arch and the oropharynx proper. The oropharynx is the posterior continuation of the oral cavity, which communicates with the nasopharynx above and the laryngopharynx below (Fig. 39-1A and Fig. 39-1B).


The palatine arch is literally a junctional area between the oral cavity and the laryngopharynx and is formed by the soft palate and the uvula above, the anterior tonsillar pillar and glossopalatine sulcus laterally, and the glossopharyngeal sulcus and the base of the tongue inferiorly.
The retromolar trigone may be included in the structures of the faucial arch (Fig. 39-2), although it is actually located within the oral cavity, the apex being in line with the tuberosity of the maxilla(behind the last upper molar); the lateral border extends upward into the buccal mucosa; medially it blends with the anterior tonsillar pillar, its base formed by the distal surface of the last lower molar and the adjacent gingivolingual sulcus. [ref: 54]

The lateral walls of the oropharynx are limited posteriorly by the tonsillar fossa and the posterior tonsillar pillar (pharyngopalatine folds). These pillars are folds of mucous membrane that cover the underlying glossopalatine and pharyngopalatine muscles. [ref: 54] Deep to the lateral wall of the tonsillar fossa are the superior constrictor muscles of the pharynx, the upper fibers of the middle constrictor, the pharyngeus and stylopharyngeus muscles, and the glossopalatine and pharyngopalatine muscles (Fig. 39-1B). The tonsillar fossa continues into the lateral and posterior pharyngeal walls. Stratified squamous epithelium covers all of these structures. The tonsil has a heavy lymphoid structure.
The tonsillar fossa and faucial arch have a rich submucosal lymphatic network that is laterally grouped in four to six lymphatic ducts that drain into the subdigastric, upper cervical, and parapharyngeal lymph nodes. Submaxillary lymph nodes may be involved in lesions involving the retromolar trigone, the buccal mucosa, or even the base of the tongue. When the upper cervical lymph nodes contain metastatic tumor, approximately 25% of patients have metastases in the midcervical lymph nodes and about 5% to 10% in the posterior cervical lymph nodes. Metastases in the low cervical chain may appear in about 5% to 15% of patients with upper cervical lymph node involvement. Lymphatic drainage into the contralateral neck is sometimes observed in tumors that extend toward the midline.
Epidemiology
Carcinoma of the tonsil and faucial arch is relatively rare, comprising less than 0.5% of all cancers in men in the United States. According to the Surveillance, Epidemiology, and End Results Report of the National Cancer Institute, in 1992 the age-adjusted incidence was 1.5 per 100,000 white men and 3.2 per 100,000 black men. [ref: 90] Carcinoma of the tonsil is three to four times more frequent in men than in women, and the incidence increases with age; these tumors are most frequently diagnosed in the sixth and seventh decades of life. Malignant lymphomas in this location usually appear in patients 40 to 60 years of age. [ref: 5]
No specific predisposing factors have been identified in patients with oropharyngeal cancer, but it is believed that excessive consumption of alcohol and a long history of smoking contribute to a greater incidence of oropharyngeal tumors. [ref: 89]
Nicholls and associates [ref: 68] reviewed 30 cases of carcinoma of the tonsil, most of them squamous cell carcinoma. All cases of squamous cell carcinoma were negative for Epstein-Barr virus, and only one of five cases of nonkeratinizing undifferentiated carcinoma was positive.
Natural History
In general, tumors of the anterior tonsillar pillar and soft palate are better differentiated and biologically less aggressive than those of the tonsillar fossa; their growth is usually slower, and they metastasize less frequently to the regional lymph nodes. In a series of 269 patients, only 40% of palatine arch lesions were larger than 5 cm in diameter, compared with 60% of other oropharyngeal lesions. [ref: 37] Moreover, 50% to 60% of patients with primary tumors in the anterior tonsillar pillar, retromolar trigone, and soft palate had clinically negative necks, in contrast to only 24% of those with tonsillar fossa primary tumors. [ref: 37]
Lesions of the tonsillar fossa tend to be infiltrative, often involving the adjacent retromolar trigone, soft palate, and base of the tongue. Perez and associates (unpublished data) found that the primary tumor was confined to the tonsillar fossa in only 5.4% of 384 patients; 65% had involvement of the soft palate, and 41% had extension into the base of the tongue. Spread to adjacent structures is shown in Table 39-1.
Tumors limited to the posterior tonsillar pillar are extremely rare. These tumors tend to spread inferiorly along the palatinopharyngeal muscle; the lymph nodes most likely to be involved are the spinal accessory group.
Tumors of the faucial arch can be superficially spreading, exophytic, ulcerative, or infiltrative. The last two types are frequently combined. They may become extensive and involve the adjacent hard palate or buccal mucosa in less than 20% of patients.
Byers and co-workers [ref: 11] described mandibular involvement in 14% of 110 patients with primary retromolar trigone carcinomas; four patients had normal preoperative x-ray films. In six of 17 patients, mandibular involvement reported on radiographs was not confirmed on pathologic examination.
Lymphatic Drainage Lindberg [ref: 49] analyzed the distribution of nodal metastases in various locations. Retromolar trigone, tonsillar pillar, and soft palate lesions have an overall metastatic rate of about 45%. Initially, the most frequent site of nodal involvement is the jugulodigastric lymph node of the upper cervical chain (Fig. 39-3A). About 10% of patients have submaxillary lymph node involvement. Contralateral spread is infrequent (10%) and is usually confined to the internal jugular chain.


Tumors of the tonsillar fossa have a higher incidence of lymph node metastases (60% to 70%); most metastatic lesions are in the subdigastric lymph nodes, midjugular chain, and submaxillary lymph nodes (in lesions extending anteriorly) (Fig. 39-3B). The incidence of occult disease after preoperative irradiation is 22%, although Million and co-workers [ref: 65] estimate that the actual risk is probably closer to 50% to 60%.
The incidence of metastatic involvement of lymph nodes in the neck increases with tumor stage. In general, less than 10% of T1 lesions, 30% of T2 lesions, and 65% to 70% of T3 and T4 lesions have metastatic cervical lymph nodes. Tumors of the retromolar trigone, anterior faucial pillar, and soft palate rarely metastasize to the posterior cervical lymph nodes. However, this location is the site of nodal metastases in 5% to 10% of patients with tumors of the tonsillar fossa with anterior cervical metastasis. The lower neck is infrequently involved, although metastases in these lymph nodes are observed in 5% to 10% of patients with upper or midjugular lymphadenopathy. Contralateral lymphadenopathy in tonsillar tumors is noted in 10% to 15% of patients with positive ipsilateral lymph nodes.
Distant Metastases Merino and colleagues [ref: 64] reported on 5019 untreated patients with squamous cell carcinoma of the upper respiratory and digestive tracts, 546 of whom developed clinical evidence of distant metastases. Of 550 patients with faucial arch primary lesions, 37 (6.7%) developed distant metastases. Eighty percent of metastases appeared within 2 years of treatment. The lungs were the most common site of metastases (more than 50%), followed by bone (20%), liver (6%), and mediastinum (2.9%). Overall, for tumors in the oropharynx, the incidence of distant metastases increased with tumor stage (5.2% for T1, 9.6% for T2, 12.7% for T3, and 16.1% for T4 tumors). There also was an overall correlation between the incidence of nodal metastases and metastatic spread; patients with N0 or N1 cervical lymph nodes had a 5% to 12 incidence of distant metastases, but the rate was 21.8% for N2 and 27.1% for N3 lesions.
Chung and Stefani [ref: 15] reported that 72 of 471 patients (15%) with carcinoma of the tonsillar region developed distant metastases. In a subgroup of 115 patients who underwent autopsy, the incidence was 29%. Although squamous cell carcinoma was the most frequent tumor type, only 14% of these patients (58 of 416) developed distant spread in contrast to 54% (seven of 13) of those with lymphoepithelioma and 26% (five of 19) diagnosed with "transitional" cell carcinoma. Forty-six of 288 patients (16%) with lesions originating in the tonsillar fossa developed metastases, compared with 10 of 111 (9%) with lesions originating in the tonsillar pillars. The sites in 42 patients with single-organ metastatic involvement and 30 with two or more sites are illustrated in Fig. 39-4.

Clinical Presentation
These patients may present with a variety of symptoms, but the most frequent is a sore throat. They also may complain of difficulty in swallowing or pain in the ear, which is related to the anastomotic-tympanic nerve of Jacobson (Fig. 39-5).

Carcinomas of the tonsil are usually ulcerated and are sometimes exophytic (Fig. 39-6).

They infiltrate the glossopharyngeal sulcus and base of the tongue, many times with little or no mucosal involvement. Trismus may be a late manifestation of the disease if the masseter or pterygoid muscle is involved. It is common for patients with tonsillar lesions to notice a mass in the cervical region, usually subdigastric (jugulodigastric), as the first manifestation of disease. Initially, distant metastases are extremely rare.
Diagnostic Workup
A complete history and physical examination always begin the evaluation of these patients (Table 39-2). The next step is a complete examination of the head and neck, including oral cavity, oropharynx, nasopharynx, hypopharynx, and larynx, with particular emphasis on detecting abnormalities in the anterior faucial pillar, buccal mucosa, retromolar trigone, soft palate, or uvula. Mirror examination of the nasopharynx, hypopharynx, and larynx should be performed to detect any tumor extension or associated pathology.
After indirect laryngoscopy, careful digital examination with a gloved finger always should be performed to detect submucosal involvement of the glossopalatine sulcus, base of the tongue, buccal mucosa, or lateral pharyngeal wall. Direct laryngoscopy under anesthesia is seldom required for carcinoma of the faucial arch, but it is very useful to evaluate patients with larger tonsillar lesions.
Physical examination should include a thorough evaluation of the neck for detection of metastatic lymph nodes as well as a search for distant metastases. Examination of the neck should be performed with the physician standing behind the seated patient. Anatomic position, size, consistency, tenderness, and mobility of palpable cervical lymph nodes should be recorded.
Histologic confirmation of a clinically suspicious malignant lesion must always be attained, and multiple biopsies should be performed, preferably at the margins of the tumor. Incisional or punch forceps biopsies can be performed with local anesthesia on an outpatient basis. When a lymphoma is suspected, the lesion may be submucosal; a large amount of tissue may be required for electron microscopy and immunologic typing of the tumor.
Complete blood counts, chemistry profiles, and urinalysis should be obtained.
Plain films of the soft tissues of the neck or mandible may be taken if involvement of soft tissues or bony structures is suspected. Lateral soft tissue films of the neck may show extension into the posterior pharyngeal wall. Computed tomography (CT) is particularly helpful in delineating the tumor and excluding involvement of the mandible or extension into the base of the skull (Fig. 39-7).

Chest x-ray films should be routine. Bone scans should be requested only if bone involvement is suspected. X-ray films of the skeleton may be
required in patients with positive bone scans or clinical suspicion of bony lesions.
Staging
In staging these tumors, it is extremely important to include both the ulcerated and infiltrating components of the tumor and all of its submucosal extensions. Because of a tendency to overestimate the size of oropharyngeal tumors, a ruler or caliper must be used to measure the diameter of the lesion. [ref: 65] Visual, palpatory, and radiographic findings are critical in accurate staging. The usual staging classification for carcinoma of the oropharynx, including lymph node involvement of the American Joint Committee (AJC), [ref: 7] is shown in Table 39-3 and Fig. 39-8.

Pathologic Classification
These tumors have characteristic features, including keratin in many cases, although occasionally they can be nonkeratinizing. The tumors can be graded I to IV, depending on the degree of differentiation. Carcinomas that arise in the faucial arch, usually of the squamous cell type, tend to be keratinizing and more differentiated than tumors that arise from the tonsillar fossa.
Carcinomas of the tonsil usually are of the well to moderately differentiated (approximately 50% of patients) squamous cell type, but the proportion of patients with less differentiated tumors is greater than that for tumors of the faucial arch. Although it has been suggested that keratinizing, more differentiated tumors have a somewhat better prognosis than others, no definite correlation between histologic type and pattern of behavior or response to therapy has been reported. [ref: 80] "Transitional cell carcinoma" is an archaic term that formerly was used to describe poorly differentiated, nonkeratinizing squamous cell carcinomas.
Lymphoepithelioma is much rarer in the tonsil (less than 1.5%) than in the nasopharynx. Most pathologists now agree that lymphoepithelioma represents a poorly differentiated, nonkeratinizing squamous cell carcinoma with a profuse lymphoid infiltration. The classic appearance of the tumor is represented by cores and nests of moderately large, sometimes clear epithelial cells, the nuclei of which often contain one or more large nucleoli. Scattered among these masses are multitudes of lymphocytes, which probably are interspersed with the epithelial component of the tumor. [ref: 2,54]
Malignant lymphomas, usually non-Hodgkin's type, constitute 10% to 15% of malignant tumors of the tonsil. According to the Rappaport classification, they may be equally divided between small and large cell types. They tend to grow submucosally and may reach large size without significant mucosal ulceration (Fig. 39-6). The surface of the tumor is covered by the same mucous membrane that covers the soft palate. Primary Hodgkin's disease in the tonsil is extremely rare.
Tumors of the salivary gland type are uncommon in the tonsil or faucial arch. Spiro and associates [ref: 84] found only 11 of 345 tumors of the minor salivary glands of the oral cavity in this location. Malignant melanomas of the tonsillar fossa constituted 6% of melanomas found in the upper passages by Conley and Pack. [ref: 16]
Koss and associates [ref: 42] and Abedi and Sismanis [ref: 1] reported on a few patients with primary small cell carcinoma of the tonsil, with neurosecretory granules demonstrated by electron microscopy. As in other locations, this tumor has a high propensity for regional, nodal, and distant metastatic spread with a very poor prognosis.
Metastatic carcinoma of the palantine tonsil is rare, with only 92 cases reported in the world literature. Low and co-workers [ref: 52] reported a case of tonsillar metastasis from the colon.
Prognostic Factor
Several prognostic factors have been described. Gender may play a role in outcome. Oreggia and colleagues, [ref: 71] reporting the 5-year survival rates among 769 patients with carcinoma of the tonsil, found that women had a better prognosis than men (40% and 9%, respectively). In contrast, Vallis and associates [ref: 91] observed no significant survival difference between the genders.
In some studies, there is no difference in the survival rate for patients younger or older than 40 years at the time of diagnosis. Johnston and Byers [ref: 38] reported a 5-year survival rate of 14% (significantly below the overall adult rate) in 11 patients under 40 years of age. Ninety-one percent of patients had neck node metastasis; 55% were stage N3. Five of 11 patients (45%) had T3 or T4 primary tumors, and all of these died, four with regional failures. Five of six patients with N3 cervical lymph nodes died, all but one with regional failure.
A significant correlation has been found between the stage of the primary tumor, the presence of involved cervical lymph nodes, and 5-year survival. [ref: 29,74] Tumor extension into the base of the tongue is associated with decreased survival (Table 39-4). [ref: 80,81,92]
There is no definite correlation between histologic type or degree of tumor differentiation and patient survival. [ref: 80,91]
In patients treated surgically after irradiation, more than 90% with negative histologic specimens survived for 5 years compared with 30% of patients with persistent tumor. [ref: 75]
Patterns of Failure Lindberg [ref: 48] and Perez and associates [ref: 74] reported failure rates after irradiation of the tonsillar area of 5% to 30% in stage T1, 10% to 40% in stage T2, and 27% to 50% in stages T3 and T4. In approximately half of the patients, primary failure was combined with nodal metastases. The incidence of recurrences in the neck was 10% for stage N0 and N1, 25% for stage N2, and 35% to 40% for stage N3. Figure 39-9 illustrates the incidence of neck failure after combined surgery and irradiation or irradiation alone in 384 patients treated at Washington University.

Merino and associates [ref: 64] reported a 17.4% incidence (four of 23 patients) of distant metastases in the oropharynx proper after preoperative irradiation and 27.8% (five of 18) with postoperative irradiation.
In the faucial arch the incidence of distant metastases was 5% to 7% in more than 500 patients treated with irradiation or surgery and 8% to 14% in patients treated with preoperative or postoperative irradiation. Distant metastasis is correlated with the stage of the primary tumor and lymph node metastasis (Table 39-5). The overall incidence is approximately 15% for patients treated with irradiation or surgery. [ref: 48,64,74]
More than 85% to 90% of the locoregional recurrences and distant metastases take place within the first 3 years after therapy. [ref: 26,74,99]
General Management
Tumors of the Tonsil Patients with T1 or T2 carcinoma of the tonsil can be treated with irradiation or surgery alone. In general, the surgical procedure requires a radical tonsillectomy and, for T2 to T4 tumors, partial removal of the mandible and ipsilateral neck dissection. Jesse and Fletcher [ref: 37] stated that in patients with N0 necks it may not be necessary to perform elective neck dissection because of the low incidence of metastases to cervical lymph nodes in T1 and even T2 lesions (10% and 25%, respectively). Because of comparable tumor control both at the primary site and the neck, irradiation is the preferred treatment at many institutions. [ref: 22,65]
With surgery alone, Whicker and associates [ref: 97] reported failure rates as low as 20%, but others such as Terz and Farr [ref: 87] have described local failure rates as high as 41%. Maltz and co-workers [ref: 56] noted an absolute survival rate of 56% and a determinate survival rate of 67% in 36 patients with carcinoma of the tonsil treated with preoperative irradiation (40 to 45 Gy) and en bloc resection of the primary tumor and neck dissection. The survival rate was 80% for patients with T1 lesions, 68% for T2 lesions, and 33% for T3 lesions.
In T3 and T4 tumors, a combination of irradiation and surgery has been advocated because of the higher incidence of recurrences with either modality alone. [ref: 29,74] To ensure adequate surgical margins in patients who receive preoperative irradiation, it is imperative to define the scope of the operation with accurate anatomic drawings of the lesion and tattooing of the initial tumor extent.
Preoperative doses of 30 to 50 Gy in 3 to 5.5 weeks have been administered to the primary tumor and ipsilateral (or both) necks. [ref: 74] At Washington University, extensive lesions (T3 and T4) are treated with a surgical procedure, if feasible (radical tonsillectomy with ipsilateral neck dissection), followed by postoperative irradiation (50 to 60 Gy), depending on the status of the surgical margins and extent of cervical lymph node involvement.
Many patients with tonsillar tumors, particulary T1, T2, and T3, are treated with irradiation alone (60 to 75 Gy in 6 to 8 weeks, depending on stage). Regional lymph nodes are treated with 50 Gy (subclinical disease) to 75 Gy, depending on nodal involvement.
Tumors of the Faucial Arch T1 lesions less than 1 cm in diameter can be treated with wide surgical resection or irradiation alone (60 to 65 Gy in 6 to 7 weeks). T2 or larger tumors require more extensive surgical procedures, including partial resection of the mandible if there is bone involvement. Because of the tendency of these tumors to extend to the midline, the site of lymph node metastasis is less predictable; therefore, neck dissection should be performed only in patients with palpable cervical lymph nodes. These tumors also can be treated with irradiation alone (65 to 70 Gy); radiation therapy has the advantage of treating subclinical disease in the neck (50 Gy total dose).
In more extensive lesions, preoperative or postoperative irradiation can be used in doses similar to those used in the tonsil. Million and co-workers [ref: 65] noted that combined therapy for lesions of the soft palate is rarely used because of the success rate with irradiation alone and the morbidity associated with resection of the soft palate.
Radiation Therapy Techniques
Volume Treated In general, the same portals and doses of irradiation can be used for the treatment of tumors of the tonsillar region or the faucial arch, depending on the stage of the primary tumor and the lymph nodes. The standard arrangement consists of opposing lateral portals that include the primary tumor, adjacent tissues (i.e., buccal mucosa, gingiva,base of the tongue, distal nasopharynx, and lateral/posterior pharyngeal wall), and the upper and posterior cervical lymph nodes
(Fig. 39-10).
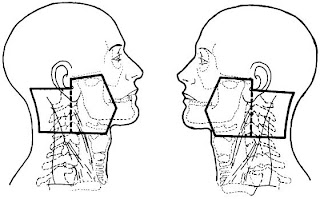
The external landmark for the upper margin is the zygomatic arch and, on x-rays, the floor of the sphenoid sinus. The middle and internal ear should be carefully shielded posteriorly, making sure that tumor volume is not covered. The portal extends posteriorly around the external auditory canal to a line joining the tip of the mastoid to about 1 cm above the foramen magnum. The anterior margin should be set up by clinical examination (inspection and palpation of the buccal mucosa and base of the tongue) with at least a 2-cm margin beyond any clinical evidence of disease. This margin should project 2 to 3 cm forward of the anterior cortex of the ascending ramus of the mandible, depending on tumor extent. The portal should also include the submandibular nodes if there is buccal mucosal involvement. Inferiorly, the portal extends to the thyroid notch, except in patients who have downward tumor extension with pharyngeal wall involvement, in which case the margin must be placed below that level (Fig. 39-11).

Posteriorly, the posterior cervical lymph nodes should be covered; a small amount of subcutaneous tissue should be spared to avoid fall-off, except in patients with palpable posterior cervical lymph nodes.
After a tumor dose of approximately 43 to 45 Gy, the posterior margin of the lateral portal is brought anteriorly to the midportion of the vertebral bodies to spare the spinal cord. Examples of simulation and localization films for reduced portals (excluding the spinal cord) are illustrated in Fig. 39-12.

If desired, doses higher than 45 Gy may be delivered to the posterior necks with lateral electron beam portals (9 MeV) or, if photons are used, with posterior appositional fields, shielding the spinal cord with a midline block. After a minimum total tumor dose of 60 Gy has been delivered to the oropharynx, depending on the extent of the tumor, the portals may be concentrically reduced by to 2 cm, and additional dose is delivered to complete the 65- to 75-Gy total dose (Fig. 39-13).

Compensating filters (Ellis type), designed with the central axis of the field as the point of reference, are used with the upper neck lateral portals to compensate for a varying contour and thickness of the neck in the superior-inferior as well as in the lateral directions.
At Washington University, after portal reduction for shielding of the spinal cord, the Cerrobend block is filled posteriorly and the central axis remains unchanged, allowing the compensating filters initially constructed to be used for the later part of the treatment.
It is not necessary to treat the posterior cervical chain or the midlower cervical lymph nodes in T1N0 tumors; smaller portals are adequate (Fig. 39-14A and Fig. 39-14B).


Murthy and Hendrickson [ref: 67] pointed out that the probability of contralateral lymph node failure is less than 10% in patients with N0 and N1 tonsillar tumors with controlled primary tumor and ipsilateral neck disease, questioning the need for irradiation of the contralateral upper cervical lymph nodes in these patients. Limiting irradiation to the primary tumor and ipsilateral neck reduces the probability of xerostomia.
The lower neck is treated with a standard anteroposterior portal. If no palpable lymph nodes are present, a 5 half-value layer 1.5- to 2-cm wide midline block can be used to shield the larynx and spinal cord. However, if lymph nodes are involved in this area, only a small block to shield the larynx and a portion of the spinal cord (to avoid overlap with the lateral portals) is used (Fig. 39-15).

The various portals used in the treatment of a patient with a T2N1M0 epidermoid carcinoma of the left tonsil are illustrated in Fig. 39-16.

A technique described by Fletcher [ref: 22] for treatment of small tumors of the tonsillar fossa, anterior tonsillar pillar, and retromolar trigone used ipsilateral wedged angle anterior and posterior fields that irradiated a triangular volume with the base on the neck and the apex in the uvula (Fig. 39-17).

With this technique the dose to the mandible is high; as with unequally loaded fields with low-energy photons, a greater incidence of complications (e.g., soft tissue necrosis and osteonecrosis of the mandible) was observed, [ref: 30] but this was not substantiated in a later analysis of 676 patients. [ref: 98]
Doses of Irradiation Alone Tumor doses are usually calculated at the midline of the upper necks. For T1 tumors, minimal doses of 60 to 65 Gy should provide local tumor control in over 90% of patients. For T2 tumors, 65 to 70 Gy is necessary, and for T3 and T4 tumors, 70 to 75 Gy is needed to improve local tumor control. Shrinking fields must be used with doses beyond Gy to decrease the incidence of complications. Because of the limited tolerance of the normal tissues (e.g., mandible, salivary glands, and even the subcutaneous tissues), it is not advisable to administer tumor doses over 75 Gy with external megavoltage beams.
The upper neck should receive 46 to 50 Gy for N0 (subclinical) disease, 65 Gy for N1 and N2 nodes, and up to 70 to 75 Gy for N3 lymph nodes. This can be accomplished with reducing fields and delivery of boosting doses with 12- to 16-MeV electrons (Fig. 39-18).

If there are no palpable lymph nodes, the minimum tumor dose delivered to the posterior and lower necks is 45 Gy (calculated at 3 cm).
Standard daily fractionation is 1.8 to 2 Gy, five fractions per week.
Preoperative Irradiation When preoperative irradiation is used for large primary tumors with involved cervical lymph nodes, doses of approximately 40 to 45 Gy in 4 to 5 weeks are delivered. The patient is evaluated for operability, and, if possible, a radical surgical resection with neck dissection is performed. Otherwise, additional irradiation is given to achieve a total tumor dose of 70 to 75 Gy.
Postoperative Irradiation In the past 15 years, postoperative irradiation has gained popularity. For T2N0 tumors with negative surgical margins, tumor doses of 50 Gy
in 5 to 6 weeks to the primary site and both necks should suffice. For more extensive primary tumors or for cervical lymph node involvement, Gy in 6 to 7 weeks is delivered. If positive surgical margins, extracapsular nodal extension, or more than three metastatic lymph nodes exist, an additional 5 to 10 Gy is given with reduced portals using 12- to 16-MeV electrons. Interstitial brachytherapy can be used for this purpose.
Guidelines for treatment are summarized in Table 39-6.
Altered Fractionation Marcial and colleagues [ref: 58] used split-course irradiation for treating patients with tonsillar tumors and for other head and neck malignancies in a randomized Radiation Therapy Oncology Group (RTOG) study. Patients received a total dose of 3 Gy daily for 10 fractions in 2 weeks, 3 weeks of rest, and an additional total dose of 30 Gy in 3-Gy daily fractions, 5 days per week. A control group was treated with 60 to 66 Gy with 2- to 2.2-Gy fractions. The complete response rate was 57% in 63 patients treated with split-course therapy versus 61% in 74 patients receiving continuous-course irradiation.
Locoregional control of tumor at 5 years was 25% for split-course and 28% for continuous therapy; the rates at 7 years were 25% and 24%, respectively. Absolute survival in the split-course patients tended to be lower than in the other group. Acute and late tissue reactions were the same in both groups. The compensated split-course technique yielded clinical results equal to those of conventional continuous therapy, with the advantage of requiring fewer radiation fractions and less burden on the patient and therapy facilities.
Mendenhall and colleagues [ref: 63] and Wang [ref: 93,94] used multiple daily fractionation to increase the overall dose of irradiation without enhancing morbidity. Wang [ref: 93] described higher tumor control and survival in 52 patients with tumors of the tonsil and 47 with base of the tongue carcinoma treated with twice-daily fractionation to total doses of 67.2 Gy than in 71 historic controls with similar tumors treated with one daily fraction of 1.8 Gy to doses of 65 Gy. In an update, Wang and associates [ref: 95] reviewed 162 patients with T3 squamous cell carcinoma of the oropharynx and larynx treated with accelerated hyperfractionation (1.5 to 1.6 Gy two or three times daily); they reported 3-year tumor control rates of 80% in patients with mid- course treatment gaps of less than 14 days (32 of 80 patients) compared with 58% (27 of 82) with longer interruptions in therapy. The local tumor control rate was 77% for patients treated in fewer than 45 days (38 of 91 patients) and 57% with longer treatment periods (P = 0.0076). Total dose was also a factor in local tumor control (83% for patients receiving 70 Gy or greater versus 65% for patients receiving doses lower than 67 Gy) (P = 0.048).
Horiot and colleagues, [ref: 34] in a randomized European Organization for Research on Treatment of Cancer study of 325 patients with stage T2 and T3 orpharyngeal carcinoma, observed better local tumor control and survival (59% and 47%, respectively, at 5 years) in 159 patients treated with hyperfractionation (80.5 Gy in 70 fractions, 1.15 Gy twice daily, in 7 weeks). This group was compared with 166 patients treated with single daily fractions of 2 Gy (70 Gy, 35 fractions, in 7 weeks) in whom 5-year local tumor control was 40% (P = 0.02) and survival was about 31% (P = 0.08).
Beam Energy An optimal energy for the treatment of the cervical lymph nodes is
**60Co, 4- or 6-MV photons. These beams also can be used for irradiation of tonsillar faucial arch primary lesions and extensions, including the base of the tongue. However, with a 60-Gy midline dose, the mandible receives 65 to 70 Gy total dose. At Washington University, after a 43- to 45-Gy tumor dose, high-energy photons (18 MV) are frequently used in patients without palpable neck nodes to achieve a high midline dose with relative sparing of the superficial tissues, the temporomandibular joint, and the mandible. Figure 39-19 illustrates the difference in dose to the mandible using low- or high-energy photons for the last 20 Gy of therapy.

Electrons ranging from 12 to 20 MeV can be used to boost the dose to the primary tumor or large cervical lymph nodes. If necessary, the posterior cervical nodes are irradiated with 9-MeV electrons. The lower neck is treated with **60Co, 4- or 6-MV photons, without any difficulty.
Intraoral Cones The intraoral cone technique, using orthovoltage or electrons, has been selectively used in the treatment of patients with small lesions. [ref: 38,80]
Brachytherapy Fletcher and associates [ref: 24] advocated the use of a single- or
double-plane pterygopalatine implant for treatment of patients with carcinoma of the tonsil or palatine arch when external irradiation was not satisfactory. Later, Amornmarn and associates [ref: 2] and Mazaron and colleagues [ref: 61,62] described similar techniques. This approach can be used to treat recurrent tumors (Fig. 39-20).

Results of Therapy
Some modern clinical radiation biology concepts are based on Coutard's study [ref: 17] of patients irradiated for tumors of the tonsillar region. He made landmark observations on the effects of radiation on normal tissues, the correlation of doses of irradiation and probability of tumor control, and the importance of the dose-time relationship in the prevention of treatment complications.
Tonsillar Fossa Irradiation Alone Radiation therapy yields a high probability of tumor control in T1 (85% to 90%) and T2 tumors (70% to 80%). In T3 and T4 lesions, tumor control rates are 60% and 40%, respectively [ref: 70] (Table 39-7).
Million and co-workers [ref: 65] described results in 99 patients treated with irradiation (60 to 70 Gy) and surgery for salvage of failures; the determinate 5-year survival rates were 100% for stage I, 90% for stage II, 75% for stage III, and about 26% for stage IV. Mendenhall and associates [ref: 63] reported their experience with 104 patients who received irradiation alone and 32 treated with a combination of irradiation and neck dissection; Lee and colleagues [ref: 46] updated their report on 243 patients with squamous cell carcinoma of the tonsillar region treated with radiation therapy. The respective initial and ultimate tumor control rates (including surgical salvage) were 87% and 100% for T1, 79% and 92% for T2, 71% and 76% for T3, and 44% and 48% for T4. Multivariate analysis demonstrated that anterior extension of the primary tumor (P = 0.0001)
and T stage (P = 0.014) were the most significant parameters affecting local control after radiation therapy. For T4 lesions, twice-daily irradiation significantly improved local tumor control (P = 0.04). The 5-year absolute and cause-specific survival rates using the modified AJC stages were 37% and 100%, respectively, for stage I, 55% and 90% for stage II, 55% and 85% for stage III, 35% and 60% for stage IVA, and 23% and 38% for stage IVB. The incidence of severe complications was 3% for the entire group of patients.
Fein and co-workers, [ref: 21] in an update of their experience, reported equivalent local tumor control in similar-stage patients treated for carcinoma of the tonsillar region (250 patients) or soft palate (92 patients) with once- or twice-daily fractionation. Median doses were 68 Gy (1.7 to 2 Gy once daily) or 76.2 Gy (1.2 Gy twice daily). Results are summarized in Table 39-8. In a study of 150 patients, Wong and associates [ref: 101] noted excellent tumor control in T1 (94%), T2 (74%), and T3 (58%) lesions with irradiation alone. Determinate 5-year survival rates were 100% for stage I, 80% for stage II, 74% for stage III, and 60% for stage IV. The incidence of severe complications in 137 patients treated with conventional fractionation was 4% with less than 67.5 Gy and 18.6% (16 of 86) with higher total doses.
Comparable results have been described by Fayos and Lampe, [ref: 20] Nussbaum and associates, [ref: 69] Wang, [ref: 92] and Mizono and colleagues. [ref: 66] Mendenhall and co-workers [ref: 63] and Perez and colleagues [ref: 75] noted that doses of 60 to 65 Gy are adequate to control T1 lesions, and 70 Gy is sufficient for most T2 tumors delivered with 1.8 to 2 Gy per day in five weekly fractions, whereas T3 and T4 tumors are locally controlled in 60% of patients receiving 70 to 75 Gy.
We observed a lack of dose response in tumor control for the primary tumor or the lymph nodes in our patients; this does not contradict reports showing a correlation between dose and tumor control because it is our practice to deliver higher doses of irradiation to larger tumors and to those showing a lesser response toward the end of the prescribed therapy. Other investigators confirm our experience; Cardinale and Fischer [ref: 12] noted 100% tumor control in 13 T1 lesions with doses of 50 to 65 Gy and in two instances with doses as low as 42 Gy. Only two of 16 T3 lesions were controlled with 60 to 70 Gy. Garrett and colleagues [ref: 26] did not observe a significant correlation of tumor control in 372 patients treated with irradiation doses ranging from 50 Gy (delivered in daily fractions of 2 or 2.5 Gy) to 60 Gy (2-Gy fractions), but there was a statistically significant improvement in local tumor control and survival when areas greater than 80 cm**2 were treated in T1 and T2 tumors.
Among 215 patients with tonsillar region carcinomas, Dubois and associates [ref: 18] noted a correlation of tumor control with larger volumes treated but not with increasing nominal standard dose. Similarly, Gelinas and Fletcher, [ref: 28] in an analysis of 155 patients with tonsillar carcinoma, demonstrated that failure to control the tumor was related to geographic miss in five patients and lower doses in seven patients, although they found no obvious reason for 11 failures. Another report from Washington University [ref: 75] indicated that inadequate doses of irradiation were correlated with the inability to control the tumor in approximately 10% of patients with T1 and T2 tumors and 20% with T3 and T4 lesions. A combination of inadequate portals with geographic misses and lower doses of irradiation was noted in an additional 10% of patients with small lesions and 20% of those with T3 and T4 tumors.
Bataini and associates, [ref: 6] in a multivariate analysis of 465 patients with tumors of the tonsillar region (including the pillars and glossopalatine sulcus) treated with irradiation alone (65 to 68 Gy in 6 to 7 weeks), noted that the stage and site of the primary tumor were the only significant prognostic factors influencing tumor control. The length of overall treatment time was the only technical variable associated with local control. Patients with tumors of the tonsil and anterior or posterior tonsillar pillar had better 3-year tumor control (72% and 66%, respectively) than those with tumors in the glossopalatine sulcus (48%).
Gwozdz and colleagues [ref: 32] described results in 82 patients with carcinoma of the tonsil who received a concomitant boost (second daily fraction of 1.5 Gy) during the last 2 to 2.5 weeks of radiation therapy. Median dose to the primary tumor was 72 Gy, and median duration of treatment was 42 days. With a median follow-up of 42 months, the local tumor and locoregional control rates were 83% and 76%, respectively. The tumor control rates were 100% for T1, 96% for T2, 78% for T3, and 25% for T4 tumors. The 5-year disease-specific survival rate was 68%. Grade 3 or 4 mucositis occurred in all patients. Median weight loss was 18 pounds, and 15 patients required feeding tubes. Seven patients had mucosal sequelae, four had bone complications, and two developed chronic dysphagia; one mandibular osteosarcoma was observed 8 years after treatment.
Withers and associates [ref: 99] published a survey of 676 patients with carcinoma of the tonsillar fossa treated at nine institutions with doses ranging from 50 to 72 Gy, dose per fraction of 1.8 to 3.3 Gy, and overall treatment time of 3 to more than 8 weeks. The follow-up rate at 3 years was 97.1% and at 5 years, 84%. Local recurrence rates were 10% to 20% for T1, 25% for T2, 40% for T3, and 50% for T4 tumors. Local tumor control was higher in patients with negative lymph nodes and increased by nearly 2% for each 1-Gy increase in total dose. For a constant total dose there was a decrease in local tumor control with prolongation of overall treatment time, presumed to result from accelerated regrowth of surviving tumor clonogens during the course of irradiation. It is assumed that this accelerated regrowth began within 9 days of start of treatment and occurred at a constant rate, with an average of 0.53 Gy extra dose per day required to maintain a constant probability of tumor control. Because of the assumed high alpha/beta ratio for this tumor, the dose per fraction was not a significant factor. There was at least a 1% per day decrease in tumor control probability when overall treatment time was prolonged, requiring a compensatory increase of 0.5 to 0.7 Gy per day.
Combined Irradiation and Surgery Combined therapy may be more effective in patients with more extensive tumors (T3, T4, or clinically palpable neck nodes), who have a lower probability of tumor control with irradiation alone, or in patients with persistent tumor after initial definitive irradiation. To improve tumor control therapy in these selected patients, higher doses of irradiation combined with surgery should be given (45 Gy preoperatively or 60 Gy postoperatively). Both approaches are equally effective.
Perez and colleagues [ref: 74] reported results of therapy in 384 patients with carcinoma of the tonsillar fossa treated at Washington University: 154 received irradiation alone (55 to 70 Gy), 144 received preoperative irradiation (20 to 30 Gy) or were initially planned for preoperative irradiation but were treated with radiation therapy alone, and 86 were treated with postoperative irradiation (50 to 60 Gy). The surgery in all except four patients consisted of en bloc radical tonsillectomy with ipsilateral lymph node dissection. Actuarial 5-year disease-free survival was 76% for T1 tumors, 54% for T2, 45% for T3, and 20% for T4 tumors (Table 39-9). There was no significant difference in the results with irradiation alone or sugery combined with preoperative or postoperative irradiation. The locoregional recurrence rate was about 25% for T1, T2, and T3 tumors and 50% for T4 lesions. The neck failure rates were 10% for N0 and 25% to 37% for N1, N2, and N3 nodes. Results are shown in Fig. 39-21AB and Fig. 39-21C.


Mantravadi and co-workers [ref: 57] described results with radiation therapy alone (65 to 70 Gy) for 94 patients and combined surgery and irradiation (20 to 50 Gy) for 23 patients. Survival and tumor control at the primary site or in the necks for both treatment groups were similar to those noted at Washington University.
Barrs and colleagues [ref: 4] reported on 119 patients with carcinoma of the tonsil and base of the tongue treated primarily with surgery alone (67 patients, most with T1 or T2 tumors), combined operation and irradiation (25 patients), or irradiation alone (remainder of patients). In the surgical group, the 3-year survival rates were 63% for patients with T1 lesions, 56% for patients with T2 lesions, and 31% for patients with T3 or T4 lesions. With irradiation alone the 3-year survival rates were 68% for stage T1 patients, 52% for stage T2 patients, and 38% for the T3 patients. The differences are not statistically significant.
Kajanti and Mantyla [ref: 40] reported on 75 patients treated for squamous cell carcinoma of the tonsillar region; 30 received combined surgery and postoperative irradiation, and 45 were treated with radiation therapy alone. The radical irradiation group included more patients with advanced-stage disease (27% stage III and 66% stage IV) than did the combined-therapy group (47% and 23%, respectively). The 5-year survival rates were 39% for the entire patient series, 53% with combined therapy, and 29% with radical irradiation.
Mizono and associates [ref: 66] described better locoregional tumor control (23 of 34 patients, 68%) with combined irradiation and surgery compared with a group of patients with similar T3-4N1-3 tumors treated with irradiation alone (50 of 131 [38%]).
Zelefsky and co-workers [ref: 102] reported results of 31 patients with squamous cell carcinoma of base of the tongue and 20 patients with tonsillar fossa carcinoma treated with surgery and postoperative irradiation. Indications for radiation therapy included stage T3 or T4 disease (34 patients [66%]), close or positive margins (33 patients [64%]), and multiple positive neck nodes (43 patients [84%]). At 7 years, local tumor control was achieved in 17 of 18 patients (94%) with T3 lesions and 12 of 16 patients (75%) with T4 lesions. With positive or close margins and doses of 60 Gy or more, the long-term control rate was 93%. Treatment interruption had a negative effect on local tumor control, which was 64% in patients who required a break and 93% in those who did not (P = 0.05). At 7 years, overall survival for all patients was 52%, and disease-free survival was 64%. The incidence of neck failure was 18% for patients with tonsillar fossa lesions. The likelihood of having distant metastasis at 7 years was 30% for all patients. Second malignancy was not observed in patients with tonsillar fossa lesions.
Gehanno and associates [ref: 27] described results in 120 patients with tonsillar carcinoma, 70 treated with primary surgery followed by irradiation and 50 with salvage surgery after failure of primary radiation therapy. Follow-up was 6 years. The 5-year actuarial survival rates were 46% after primary surgery and 24% after salvage surgery. The disappointing survival rate with salvage surgery resulted from a higher postoperative mortality rate (8%) than with primary surgery (1.4%) and from a higher local failure rate (36% and 14%, respectively). The outcome was invariably unfavorable when tonsillar tumors extended into the base of the tongue.
Thompson and colleagues, [ref: 88] in 16 patients who received postoperative adjuvant radiation therapy for squamous cell carcinoma of the tonsil, noted a 5-year overall survival rate of 74% and a disease-free survival rate of 68%. The 5-year locoregional tumor control rate was 83% for 12 patients with pathologic stage III or IV disease; the 5-year disease-free survival rate was 74%.
Foote and co-workers [ref: 25] described 56 patients with squamous cell carcinoma of the tonsil treated with surgery alone and 16 treated with surgery and postoperative adjuvant irradiation. The 5-year survival rates for patients with clinical stage III or IV disease treated with surgery and postoperative irradiation were 100% and 78%, respectively. The 5-year overall survival rates for patients with clinical stage III, IVA, or IVB disease treated with surgery alone were 56%, 43%, and 50%, respectively.
Quenelle and associates [ref: 79] described 58 patients treated with preoperative irradiation (50 Gy) followed by complete radical resection of the tumor. As in the previous series, the survival and tumor control rates were similar to those reported for other patients treated with irradiation alone. [ref: 12,18,20,28,63]
At Helsinki University, [ref: 39] 40 patients with squamous cell carcinoma of the tonsillar region were treated with surgery and postoperative split-course irradiation. The 5-year survival rates were 100% in stage I, 75% in stage II, 63% in stage III, and 15% in stage IV. The local tumor control rates were 100%, 89%, 87%, and 38% for stages I to IV, respectively. In a proportional hazards regression analysis, tumor and node category and pretreatment Karnofsky index had the strongest association with survival, whereas tumor and node stage and total irradiation dose were most strongly associated with time to
recurrence.
The RTOG studied 354 patients with advanced carcinoma of the oral cavity, oropharynx, supraglottic larynx, and hypopharynx who were randomized to receive preoperative irradiation (50 Gy, 2-Gy fractions, five times weekly) or postoperative irradiation (60 Gy to the primary tumor and 50 Gy to both necks). [ref: 43] The overall tumor control rate was slightly better in the postoperative irradiation group (65%) compared with the preoperative group (48%) (P = 0.81). In the oropharynx, the 4-year survival rates were 26% with preoperative irradiation and 38% with postoperative radiation therapy. Complications of therapy were approximately the same: 10% to 11% in the surgical group and 11% to 14% in the irradiation patients.
At Washington University, the incidence of complications was somewhat higher in patients treated with combined therapy than in those treated with irradiation alone. [ref: 74] The observed morbidity with combined therapy is comparable with that in patients with tumors of the larynx and pharynx treated at our institution with a surgical procedure alone.
Brachytherapy Pernot and colleagues [ref: 76] described 361 patients with velotonsillar carcinoma treated with either brachytherapy alone (18 patients) or combined with external-beam irradiation (343 patients). The distribution of patients according to localization was 128 tonsil, 134 soft palate, nine posterior pillar, 63 anterior pillar, and 27 glossotonsillar sulcus. Patients were staged as follows: 90 T1, 141 T2, 119 T3, two T4, and nine Tx with 230 N0, 93 N1, nine N2, 20 N3, and nine Nx. Results at 5 and 10 years showed the following distribution: local tumor control, 80% and 74%; locoregional control, 75% and 70%; overall survival, 53% and 27%; and cause-specific survival, 63% and 52%, respectively. Univariate analysis disclosed better local tumor control at 5 years for T1 and T2 tumors (87%) compared with T3 (67%) (P = 0.00004). Locoregional tumor control was better for N0 (80%) than for N+ disease (55%) (P = 0.002). The same is true for overall survival (59% versus 42%) (P = 0.002). Tumors with extension to the mobile tongue or the base had a poor prognosis (P < 0.002). Fewer recurrences occurred if the total duration of treatment was less than 55 days and the number of days between external-beam irradiation and brachytherapy was less than 20. Only the dose rate was significant for sequelae.
Amornmarn and colleagues [ref: 2] noted local tumor control rates of 94% in 16 T1 lesions, 88% in 36 T2 lesions, 62% in 42 T3 lesions, and 19% in six T4 lesions in 100 patients with tonsillar carcinoma treated with external beam and brachytherapy. Puthawala and associates [ref: 78] reported on 80 patients with carcinoma of the tonsillar fossa, 65 of whom had locally advanced tumors treated with external irradiation (45 to 50 Gy) followed by an interstitial **192Ir implant (20 to 25 Gy for T1 and T2 tumors and 30 to 40 Gy for T3 and T4 lesions). Neck masses were separately implanted to receive an additional 20 to 40 Gy. With a minimum 2-year follow-up, the overall tumor control rate was 84%, and almost 100% with T1 and T2 tumors and 65% to 70% with T3 and T4 tumors. Three-year survival was 72%. Salvage of neck and local failures was possible in 78% and 38% of patients, respectively. Soft tissue or bone necrosis occurred in 6% (five of 80 patients).
Leborgne and associates [ref: 45] noted a 60% tumor control rate in 15 patients with tongue extension treated with external irradiation and brachytherapy in contrast to 38% in 39 patients receiving external irradiation alone. On the other hand, Garrett and associates [ref: 26] found no improvement in local tumor control in 68 patients with tonsillar carcinoma extending into the glossotonsillar sulcus or base of the tongue in whom an interstitial implant was added to external irradiation; at 5 years, local control was 57% with implant and 52% without.
Behar and colleagues [ref: 9] reviewed 37 patients with squamous cell carcinoma of the tonsillopalatine region treated with external-beam irradiation (54 Gy) and an **192Ir interstitial implant (four stage I, five stage II, 10 stage III, and 18 stage IV cancers). Eighteen patients (49%) had N2 or N3 cervical lymphadenopathy. All patients received an interstitial **192Ir implant using a combination of intraoral swage and external looping technique (mean dose 27 Gy; range 20 to 40 Gy). Eighteen patients (49%) also had neck dissection. Local tumor control was obtained in 35 of 37 patients (95%); 32 (87%) have remained disease-free in the neck. Nine patients developed second primary lesions, and one showed pulmonary metastasis. Fifteen patients died (six of their cancers, six of second primary lesions, two of intercurrent disease, one of unknown cause). The 5-year actuarial
freedom from relapse was 75%, and overall survival was 64% (mean follow-up 43 months; range 5 to 110 months). Complications were limited to one case of osteoradionecrosis of the mandible and one tonsillar ulcer. Functional and aesthetic integrity were preserved in most patients.
Faucial Arch In general, tumors of the faucial arch have better tumor control and prognosis than do those of the tonsillar fossa. Fletcher and Lindberg [ref: 23] reported a failure rate of 10% or less in retromolar trigone and soft palate T1 lesions, 18% in T2 tumors, and 16% in T3 tumors. There was a slightly higher absolute 5-year survival rate in 173 patients with tumors of the faucial arch than in those with tumors of the tonsillar fossa. Barker and Fletcher [ref: 3] reported on 204 patients with epidermoid carcinoma of the retromolar trigone and anterior tonsillar pillar treated with definitive irradiation. Initially **60Co was used to deliver 60 Gy in 4 to 5 weeks through small fields for early stages. After 1963, 18-MV photons were combined with 18-MeV electrons, either for the entire treatment or as a boost after administration of 50 Gy. For T1 lesions, doses of 60 to 65 Gy in 6 to 6.5 weeks controlled over 95% of tumors; for T2 and T3 lesions a control rate of over 90% was obtained with 70 Gy in 7 weeks. Higher doses were required for T4 tumors.
In a study of 110 patients who had squamous cell carcinoma of the retromolar trigone treated with various modalities depending on tumor stage, Byers and associates [ref: 11] reported a local or regional (neck) control rate of 84% with irradiation alone. Regardless of the method of therapy, the primary tumor control rates were 92% for T1, 88% for T2, 90% in T3, and 75% for T4 tumors. The cervical lymph node control rates were 89% for N0, 86% for N1, 83% for N2, and 66% for N3 lesions.
Pourquier and colleagues [ref: 77] described 53 cases of tumors of the retromolar trigone and buccal mucosa treated with combined cobalt therapy and electrons (used on alternate days with telecobalt therapy or as a boost). Therapeutic results were satisfactory for T1 and T2 lesions (seven of eight and seven of nine, respectively). For T3 lesions of the trigone (six of 16) and especially those of the internal surface of the cheeks (two of nine), the success rate was considerably lower. In T4 lesions, palliation was obtained but without definite improvement.
Cheng and co-workers [ref: 13] published results in 21 patients with carcinoma of the anterior tonsillar pillar and 45 with tumors of the soft palate-uvula treated with external irradiation (65 to 75 Gy), external irradiation (40 to 45 Gy) followed by a radon seed implant (20 to 40 Gy, depending on the stage of the lesion), or split-course external irradiation to deliver 60 to 75 Gy in 10 to 13 weeks. The 5-year absolute survival rates were 46% to 57% for 23 T1 lesions, 35% to 75% for 24 T2 tumors, and 22% for 11 T3 lesions with the various techniques. The local recurrence rate for T1 and T2 tumors was 7.4% (two of 27 patients) with external irradiation to doses of 60 to 75 Gy, in contrast to 33% (three of nine) with 40 to 45 Gy external irradiation and a radon seed implant in the soft palate.
A retrospective study of 188 patients with squamous cell carcinoma of the soft palate, uvula, and anterior faucial pillar treated for cure was published by Weber and associates. [ref: 96] Men predominated (1.9:1); 55% of the patients were between 60 and 70 years of age. Mean follow-up was 56.7 months. TNM stage distribution was 29, 67, 37, and 49 patients for stages I, II, III, and IV, respectively; six patients were unstaged because of previous excisional biopsy. Treatment to the primary site consisted of radiation therapy (150 patients), surgery alone (28 patients), and combined therapy (10 patients). Primary tumor control rates were 91% (31 of 34), 77% (71 of 92), 77% (30 of 39), and 35% (six of 17), respectively, for stages I through IV. At presentation, 128 patients were N0, and 60 patients (32%) had regional nodal metastasis. Regional tumor control was obtained in 87.5% of patients with N0 necks and in 76% with nodal involvement; in patients with primary tumor control, these figures were 89% and 81%, respectively. The overall determinant 5-year survival rate was 67%. Tumor extension to the tongue base decreased survival. Survival was poorer among patients with midline tumors or those extending across the palatine arch (37 patients) compared with patients with unilateral primary tumors (151 patients) (P < 0.05). Despite similar tumor stage distribution, the incidence of regional nodal metastasis was 49% with midline tumors and 28% with unilateral tumors.
Horton and associates [ref: 35] reported on 45 patients treated with irradiation for squamous cell carcinoma of the soft palate (seven lost to follow-up or who had prior irradiation were excluded). Thirty-eight patients received a median dose of 70 Gy to the primary site. After a median follow-up of 48 months, initial primary tumor control was 83% for T1, 67% for T2, and 63% for T3 disease. After surgical salvage, local tumor control increased to 92%, 80%, and 75% for stages T1, T2, and T3, respectively. At presentation, 29% (11 of 38 patients) had cervical node metastases. Irradiation provided regional control in 96% of 27) with N0 disease and 86% (six of seven) with N1 disease at diagnosis. Sixteen patients (42%) had no additional malignancy of the upper aerodigestive tract.
A multicenter retrospective study of 23 tumors of the uvula less than 2 cm in diameter was reported by Har-El and co-workers. [ref: 33] Eleven patients (47.8%) had clinical or radiologic evidence of neck disease on presentation. Five of 12 patients (41.7%) who presented with negative necks eventually were found to have neck disease; eight patients had cervical recurrence. Only one patient had local recurrence. These findings suggest that attention should be directed to treatment of the neck of all patients with tumors of the uvula and midline soft palate, regardless of size.
Thirty patients with carcinoma of the soft palate were treated (22 were stage I and II) by Tandon and colleagues. [ref: 85] A curative dose of irradiation was used in 25 patients; four required surgical salvage. Another five cases were treated by combined surgery and postoperative irradiation. Seven patients had nodal metastases. Five-year disease-free survival was 65%.
Lo and associates [ref: 50] reported results in 159 patients with previously untreated squamous cell carcinoma of the anterior faucial pillar or retromolar trigone who received external irradiation, including a combination of electron beams with high-energy photons or **60Co to doses of 60 to 75 Gy (except 11 patients). In the N0 patients, as a rule, only the ipsilateral subdigastric nodes were treated electively to a dose of 50 Gy. The 5-year survival rate for the overall group was 83%. The failure rates for the evaluable patients were 29% for T1 lesions, 30% for T2, 24% for T3, and 40% for T4 lesions. After salvage surgery, which consisted of intraoral resection in one third of the patients or a composite operation in the other two thirds, the ultimate failure rate was 0% for T1 lesions, 6% for T2, 8% for T3, and 20% for T4 lesions (Table 39-10). In the whole group, 16 patients (10%) experienced neck failure with eight ultimate failures after salvage surgery. Infiltrative and ulcerated tumors had a significantly higher failure rate (35%) than did exophytic and superficial lesions (15%), but histologic grade had no prognostic significance. After radiation therapy, 30% of patients developed some degree of bone exposure, but only 5.5% (nine patients) required segmental mandibular resection. The probability of bone exposure was not dose related and more likely reflected tumor location on the mucoperiosteum.
Keus and co-workers [ref: 41] reported on 235 patients with tumors of the soft palate treated at the Institute Curie. Results of definitive irradiation were evaluated in 146 patients; 70 (48%) had T3 or T4 tumors, and 40 (27%) had clinically palpable cervical nodes. Megavoltage x-ray therapy was used in 103 cases, and in 43 with small or moderately advanced tumors, a combination of megavoltage and intraoral orthovoltage x-rays was used. The crude 3- and 5-year survival rates were 52% and 40%, respectively, and the disease-free survival rates were 59% and 53%. The local tumor control rates at 3 years were 92% for T1, 70% for T2, 58% for T3, and 49% for T4 lesions. Nodal failure was seen in 19 patients; in nine patients it was not associated with failure at the primary site, and in seven of nine it occurred marginally or outside the treatment portals. Crude 5-year
survival was 40%, and disease-free survival was 53%. Complications were observed in 16 patients, seven of them requiring surgery.
In 41 patients with previously untreated soft palate malignancies, Seydel and Scholl [ref: 82] reported a local recurrence rate of 32% (10 of 31 patients) with doses of 60 to 70 Gy.
A small group of patients with carcinoma of the soft palate and eight patients with posterior oropharyngeal wall carcinoma were treated at The Netherlands Cancer Institute. [ref: 55] Eleven patients were treated with radiation therapy and three with surgery, as single-treatment modalities. Five-year results for tumor control and overall survival were 67% and 41%, respectively.
Leemans and colleagues [ref: 47] described results in 52 patients with squamous cell carcinoma of the soft palate and anterior tonsillar pillar. Of 45 patients treated for cure, 38 were treated by surgery, followed by radiation therapy in 19 patients (50%). Five patients received irradiation only, and two were treated by other modalities such as intraarterial methotrexate and carbon dioxide (CO(2)) laser. Absolute and determinate 5-year survival rates were 62% and 77%, respectively. Sixty-four percent of patients survived 5 years recurrence free, and 27% developed multiple primary tumors in the head and neck. Tumor stages III and IV decreased survival by half compared with stages I and II. A 42% incidence of occult nodal metastases was noted.
According to Shukovsky and associates, [ref: 83] tumors of the glossopalatine sulcus are believed to arise in the tonsillar fossa, base of the tongue, or anterior tonsillar pillar. In 81 patients with squamous cell carcinoma of the glossopalatine sulcus (identified from a total group of 662 patients with tumors in the base of the tongue, tonsillar fossa, or faucial arch), 79 were followed up for more than 3 years. The failure rates at the primary site were 0% for five T1 lesions, 25% for 20 T2 lesions, 25% for 44 T3 lesions, and 41.5% for 12 T4 lesions. The 2-year relapse-free survival rates were 80% for T1 (four of five), 65% for T2 (13 of 20), 38.5% for T3 (17 of 44), and 16.5% for T4 tumors (two of 12). There was a significant correlation between the dose of irradiation and control of the primary tumor, and complications were associated with increased irradiation doses.
Brachytherapy Mazeron and co-workers [ref: 61] reviewed the results of 165 T1 and T2 squamous cell carcinomas of the faucial arch (58 T1, 107 T2, 107 N0, N1, nine N2, 19 N3) treated by definitive irradiation, some including **192Ir brachytherapy. There were 106 tumors in the tonsillar region and 61 in the soft palate and uvula. From 1971 to (period 1), only the guide gutter technique was available; implants were reserved for small tumors. Patients were managed either by definitive telecobalt therapy to the tumor site and neck node areas (group 1; n = 48; mean dose 70 Gy in five 1.8-Gy fractions per week) or by exclusive **192Ir implant (group 2, n = 11; all T1N0; 64 Gy) or by a combination of external-beam irradiation to the tumor site and neck node areas and **192Ir implant (group 3, n = 40). In 1981 (period 2), a new plastic tube technique that enabled implantation of larger areas was introduced, and all patients (group 4, n = 66) were managed by external irradiation (47 Gy) followed by **192Ir implant (31 Gy). Clinically positive neck nodes either received additional external dose with electrons or were excised. Overall 5-year survival rates were 21%, 50.5%, and 60% in groups 1, 2, and 3 and 4, respectively (P = 0.001). Five-year local tumor control rates were 58%, 100%, and 91%, respectively (P = 0.001). Five-year necrosis rates were 4.5%, 20.5%, and 18%, respectively. Comparison of results between the two periods of the study (groups 1, 2, and 3 versus group 4) shows that these two groups are statistically comparable according to site and size of tumor and nodal status and that both local control (77% versus 94% at 5 years) (P < 0.01) and disease-free survival (56% versus 71%) (P 0.03) were improved after 1980, with a trend to an increase in 5-year survival rates (42% versus 53%) (P = 0.08). Nodal control rates (86% versus 95%) and necrosis rates (11% versus 20%) were not modified. Multivariate analysis showed that both local tumor control (P < < 0.0001) and overall survival (P < 0.0001) were improved when tumor was implanted.
Esche and colleagues [ref: 19] reported on 43 patients with epidermoid carcinoma of the soft palate and uvula treated with external irradiation (50 Gy) followed by 20 to 50 Gy interstitial **192Ir using either guide gutters or a plastic tube technique. Twelve primary tumors and two recurrences after external irradiation alone were treated with an implant only for 65 to 75 Gy. Actuarial local tumor control was 92% with no local failures in 34 T1 primary tumors. The overall actuarial 5-year survival rate was 37%; the cause-specific survival rate was 64%. Only one serious complication was seen. The leading cause of death was other aerodigestive cancer, with an actuarial rate of occurrence of 10% per year.
Neutrons Neutrons alone or in combination with photons (mixed beams) have been used to treat advanced head and neck cancer. Hussey and associates [ref: 36] summarized the results of four trials at M.D. Anderson Cancer Center involving 142 patients treated on pilot studies and 95 on a randomized clinical trial. Nineteen patients with oropharyngeal tumors were included in the pilot study and 32 in the randomized trial. Nine percent of patients in the neutrons-only and 26% in the mixed-beam study developed tumor recurrence. The results for faucial arch and pharyngeal wall cancers were slightly better in the neutrons-only and mixed-beam group than with conventional treatment. However, the results for tonsillar fossa lesions were slightly better with conventional photon irradiation. The results suggested that neutron or mixed-beam therapy may be more effective than conventional irradiation in the management of regional lymph node metastasis. In the overall analysis, a significant dose-response relationship was found with neutrons, and the range of acceptable dose was narrow.
Management of Recurrences
Because the incidence of second malignancy after treatment is high and surgical salvage of treatment failures is possible, close follow-up is essential. Patients with recurrences after surgery or moderate irradiation doses should receive definitive doses of radiation therapy to the primary tumor and the cervical lymph nodes. Portals are the same as those described previously for primary management.
In patients who initially received full-course radiation therapy, radical tonsillectomy and ipsilateral neck dissection should be performed if the lesion is resectable. For failures in the neck without primary recurrence, a neck dissection is the treatment of choice. Palliative irradiation (40 to 50 Gy in 4 to 6 weeks) with external beam irradiation or brachytherapy may be used in patients with advanced recurrent disease. The volume treated should encompass the tumor with a 2- to 3-cm margin. The risk of soft tissue necrosis or osteonecrosis increases markedly. Survival is poor after a recurrence, and only a limited number of patients can be salvaged, except for localized recurrences in T1 and T2 tumors or N1 cervical lymphadenopathy.
Mazeron and colleagues [ref: 62] described 70 patients with new or recurrent oropharyngeal cancers arising in previously irradiated tissues who were treated with **192Ir afterloading implants. Actuarial 5-year local tumor control was 69%. Tumor control was strongly related to tumor size (86% for tumors less than 2 cm, 71% for 2.1- to 4-cm lesions, and 58% for 4.1- to 6-cm tumors). Although local tumor control was achieved in most patients, only 10 patients (14%) were alive at 5 years. Local control was achieved in 100% of patients with lesions of the faucial arch or posterior pharyngeal wall. Patients with lesions of the base of the tongue and the glossotonsillar sulcus had poorer results; local control was 61%.
Maulard and associates [ref: 60] reported on 28 patients, free of cervical or distant metastases, with prior irradiation of the oropharynx who underwent salvage brachytherapy for squamous cell carcinoma of the tonsil or soft palate. There were four immediate failures of radiation therapy, 14 local recurrences, and 10 new malignancies. Initial irradiation was 40 to 80 Gy to the oropharynx; mean interval between external irradiation and salvage treatment was 22 to 28 months. Salvage brachytherapy consisted of two split-course implants performed 1 month apart, delivering 35 and 30 Gy, respectively. Fifteen patients (46.5%) were clinically disease free before the second implant, and 23 (82%) were clinically disease free at the end of treatment. Five local failures were observed without any influence of tumor size, site, or histologic differentiation. Of the
four patients who had previously failed external-beam therapy, three were disease-free after salvage brachytherapy. Among 23 patients in complete remission, four (17%) developed local recurrence within a mean of 5 months. The overall local tumor control rate was 68% (mean follow-up, 41 +/- 29 months). Actuarial survival was 19% at 5 years and 30% for patients with lesions 3 cm or smaller. In 23 patients who achieved complete remission, subsequent soft tissue necrosis was observed in four cases.
Salvage brachytherapy was performed in 73 patients with velotonsillar carcinoma in a previously irradiated field. [ref: 73] There were 45 T1N0, 20 T2N0, one T3N0, one T3N2, and six TxNx tumors. The 5-year actuarial local tumor control rates were 80% and 67% for T1N0 and T2N0, respectively. The regional relapse rate was 10% in both groups. Grade 2 sequelae, not related to volume treated or dose rate, occurred in 13% of patients; no grade 3 or 4 sequelae occurred. Five-year disease-specific survival was 64%, with a plateau after the fifth year, but the 5-year overall survival was only 30%. In this series, 42% of the patients died of another carcinoma, all except two related to continued alcohol and tobacco use.
Composite resections (transmaxillary buccopharyngectomies) were performed on 134 patients as salvage treatment for local failure in patients with oropharyngeal carcinoma at the Institut Gustave-Roussy. [ref: 72] Most patients underwent some kind of supraomohyoid neck dissection. A myocutaneous flap was used in 18% of cases, which significantly reduced the rate of local complications. Early
postoperative local complications, mostly minor, occurred in 45% of patients. A new locoregional recurrence occurred in approximately half of the patients and was usually fatal. Overall survival after salvage surgery was 34% at 3 years and 23% at 5 years. The only statistically significant prognostic factor was the adequacy of the surgical margins.
Chemotherapy
Although there are no specific reports on the use of neoadjuvant or palliative chemotherapy for carcinoma of the oropharynx, the results obtained with head and neck tumors can be applied to these patients. Drugs of choice include cisplatin, alone or combined with 5-fluorouracil, and high-dose methotrexate with leucovorin rescue. [ref: 86] Bleomycin and nitrosoureas also have been used. Reports describe complete response in 40% of patients given three cycles of chemotherapy before irradiation or surgery and an additional 30% partial response, for an overall response rate of 75% or higher. Disease-free survival has been prolonged by a few months, but after 3 years no appreciable enhancement of overall survival has been
demonstrated.
The potential benefit of adjuvant chemotherapy combined with irradiation and surgery in the treatment of these advanced lesions should be further evaluated; its long-term benefit has not been documented. Agents that selectively enhance the effects of irradiation in the tumor are under investigation, such as hypoxic cell sensitizers, chemical modifiers (cytotoxic agents, halogenated pyrimidines), hyperthermia, and high linear energy transfer irradiation. [ref: 31]
Sequelae of Treatment
The most common acute sequelae after irradiation are oropharyngeal mucositis and moderate to severe dysphagia, which may cause malnutrition and jeopardize the patient's survival if drastic support measures such as gastrostomy or hyperalimentation are not taken. Severe nutritional problems occur in 5% to 10% of patients. Temporary xerostomia and loss of taste may last for several months. Marks and colleagues [ref: 59] demonstrated significant reduction in parotid gland salivary flow with doses over 30 Gy. Other complications occasionally include laryngeal edema, fibrosis, hearing loss, and occasional trismus.
The incidence of necrosis of the mandible depends on stage of tumor, dose of irradiation delivered to the mandible, use of prophylactic dental care, trauma (including dental extractions), and irradiation technique. Grant and Fletcher [ref: 30] reported severe necrosis requiring mandibulectomy in six of 88 patients (6.8%) with T1 and T2 carcinomas of the tonsillar fossa, in contrast to 13 of 88 (14.8%) with T3 and T4 tumors. The incidence of patients with bone exposure in these two groups was 29.5% and 45.4%, respectively. The incidence of osteonecrosis was higher with single homolateral fields, unilateral wedge filter arrangements, or combination of external irradiation and interstitial implants. Cheng and Wang [ref: 14] reported osteonecrosis in 13 patients who received 2000 to 2900 ret (time-dose factor of 126 to 212); this complication was rarely seen with doses below 2000 ret to the mandible. Shukovsky and co-workers [ref: 83] reported a greater incidence of mandibular necrosis with higher doses of irradiation.
Bedwinek and associates [ref: 8] noted a significant difference in the incidence of necrosis when the tumor was over or adjacent to the mandible (about 6%) or not (0%). They also described a 5.9% incidence of osteonecrosis requiring mandibular resection in 12 of 303 patients (4%) treated before 1969, when elective dental extractions were performed, and 4.5% (eight of 178) in patients on whom dental conservation was practiced.
Barker and Fletcher [ref: 3] reported a 10% incidence of spontaneous necrosis in 112 patients with T1 and T2 tumors of the retromolar trigone and anterior tonsillar pillar after doses of 60 to 65 Gy in 6 to 6.5 weeks, and a 16% incidence (nine of 57) of necrosis in patients with T3 tumors treated with 70 Gy (six of these requiring mandibulectomy). The M.D. Anderson Cancer Center experience was updated by Larson and associates [ref: 44]; of an initial population of 569 patients, 148 patients free of disease for more than 5 years were evaluated for complications. Twelve of 30 patients with faucial arch tumors and 13 of 26 with tonsillar fossa primary tumors developed osteonecrosis of the mandible, ulceration of the soft tissues, or both. Of these, five in the first group and six in the second group required mandibulectomy.
Lo and associates [ref: 50] observed a lower incidence of complications in patients with anterior faucial pillar or retromolar trigone lesions treated with unilateral electron beam and photon portals compared with parallel opposed portals delivering 50 Gy or higher (Table 39-11).
Carotid artery rupture was reported in 3% of patients in the Grant and Fletcher series [ref: 30]) and in 1% of patients analyzed by Perez and co-workers. [ref: 74]). This finding was noted in patients on whom surgery was performed for an irradiation failure.
In 144 patients treated with combined preoperative irradiation and surgery at Washington University, three patients died of carotid rupture, two of postoperative pneumonia, one of postoperative pulmonary embolus, and one of postoperative cerebrovascular accident (5% total complication rate). Other major complications included oropharyngocutaneous fistula (18 cases), osteonecrosis of the mandible (seven cases), severe dysphagia and malnutrition (seven cases), carotid rupture (three cases), and laryngeal edema (one case) (Table 39-12).
After surgical resection of more than 1 cm of tongue base, tonsil,faucial arch, and mandible on the side of the tumor and reconstruction by primary closure, high-fidelity audio recordings of conversational speech and videofluoroscopic assessment of oropharyngeal swallow showed that 11 subjects exhibited changes in speech and swallowing function postoperatively, with little subsequent improvement. [ref: 51] Patients had greatest difficulty on stop and fricative consonants and bolus propulsion.
In a later study of late normal tissue sequelae, 71 of 676 patients (11%) had severe complications involving mucosa (n = 24), bone (n = 32), or muscle (n = 21). [ref: 98] The highest actuarial incidence of complications was in the bone (12.5% at 8 years). Total dose was a significant variable (Fig. 39-22), with similar correlations observed for mucosal and muscle late sequelae.

Large dose fractions were an important factor contributing to late sequelae. The estimated alpha/beta ratio was 3.1 Gy for muscle and 0.85 Gy for bone. There were 120 patients treated with more than once-a-day fractionation for all or a portion of the therapy. The estimated relative hazard was greater than one for all three end points, suggesting that, if there is any effect of a shortened interval between fractions, it is most likely in the direction of causing greater toxicity, which is consistent with incomplete repair between fractions when half of the fractionation intervals are only 3 to 8 hours. There was a significant influence of field size on mandibular necrosis and fracture, although this was not seen for late sequelae in muscle or mucosa. This finding is consistent with the bone being composed of serially arranged functional subunits, [ref: 100] where failure in any one subunit leads to cortical fracture. There was no correlation between late complications and the use of wedges or the proportion of dose delivered with electron beam as a boost. Unfortunately, the severity of acute and late mucosal reactions could not be correlated in this retrospective analysis because of lack of reliable data on acute sequelae.
Controversial Issues
Controversy still exists as to the preferred method of treatment for T1 and T2 tumors, particularly in patients with clinically negative necks. However, because of fewer sequelae and better functional and cosmetic results, definitive radiation therapy is preferred, reserving surgery for recurrences.
T3 and T4 primary tumors are better managed with combined therapy. Postoperative irradiation may be more advantageous because of its ability to deliver higher doses to the tumor with less morbidity. However, a study by the RTOG [ref: 43] and our nonrandomized experience disclosed no significant difference between preoperative and postoperative irradiation in the treatment of oropharyngeal or tonsillar tumors.
In patients with clinically negative necks, lymph node dissection is not warranted because elective irradiation of the neck (50 Gy) controls subclinical disease in more than 95% of patients. In patients with small, mobile lymph nodes, it is possible to control the tumor with radiation therapy alone, although a radical neck dissection is equally effective. For multiple lymph nodes larger than 5 cm in diameter or fixed to the soft tissues, the preferred method of treatment is radical neck dissection and postoperative irradiation. In many instances, composite resection of the primary tumor and neck dissection can be performed, followed by radiation therapy. As noted by Mendenhall and associates, [ref: 63] the high rate of intercurrent disease deaths (25% at 5 years) in these patients precludes having a
major impact on overall survival with improvement in locoregional tumor control.
The role of adjuvant chemotherapy in patients with advanced tumors has not been elucidated.
Nessun commento:
Posta un commento